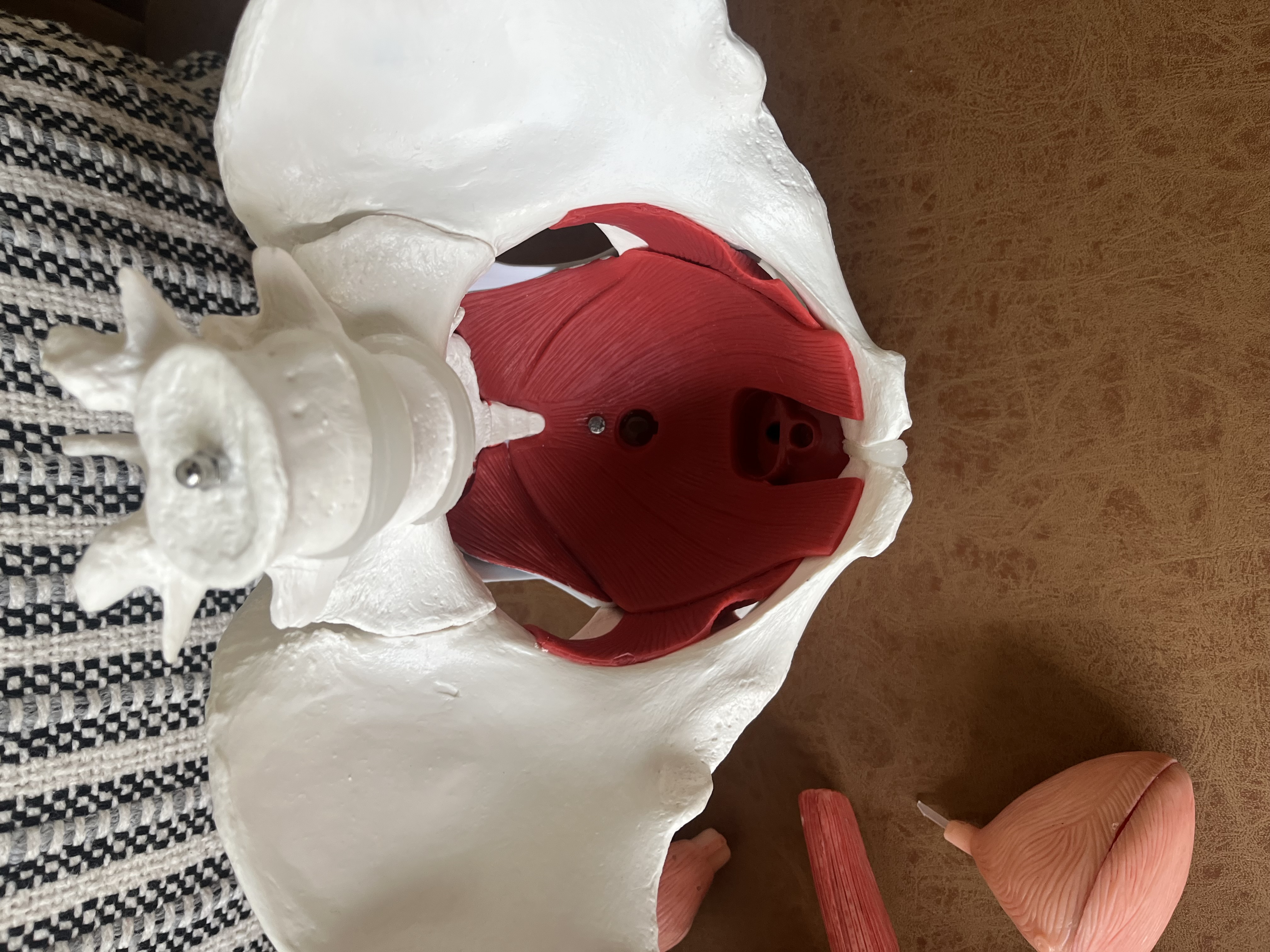
What is the pelvic floor?
A First-Time Mom's Home Birth Story (As a Healthcare Provider)
One of things that helped me the most going into birth was listening to positive birth stories - which is ultimately why I’ve decided to share mine. Negative stories tend to spread more than positive ones. Before I became pregnant I felt like all I had heard were negative pregnancy and birth stories. Because both of these experiences were positive for me, I feel all the more compelled to share. As a pelvic health physical therapist that works directly with people in their childbearing years - I feel even more obligated to use my platform to share my story.
I first think it is important to note that each pregnancy and birth experience is unique, so please don’t compare your experience to mine. I also recognize my privileges significantly contribute to my positive outcomes - which is also why I want to share what I’ve done. My privileges include my knowledge as a pelvic health PT, beginning my pregnancy being in the best shape of my life, and having the financial resources to choose the providers that aligned with my birth preferences.
My thoughts going into pregnancy
I was eager to personally implement all of my knowledge regarding pregnancy and exercise.
My husband Kelton and I used the Fertility Awareness Method to get pregnant after I was recommended the book Taking Charge of Your Fertility by Dr. Karissa Deane. I started my pregnancy journey by seeing Karissa, a naturopathic doctor, to ensure that my labs were optimal.
The book helped me learn everything about my menstrual cycle that was never discussed in health class! I would highly recommend this resource for anyone who wants to learn more about their cycle.
While it is common to have new pains during the 9-months that you grow a human, your pre-pregnancy injury baseline can significantly impact how you feel during pregnancy. Like I do with my clients that I work with to prep their bodies for pregnancy - I assessed my orthopedic injury history to make an initial exercise plan.
My most significant orthopedic issues pre-pregnancy included: lower back, left sacroiliac joint (SI joint), and left hip labrum issues while hurdling in college. In the 7 years post-college these issues would occasionally creep in when I had periods of decreased activity, but they were always well managed with regular strength training. Starting crossfit at Misfit Gym in Portland about a year before trying to get pregnant was one of the additions that helped me go into my pregnancy strong and pain-free.
My main orthopedic worry pre-pregnancy was my strange xiphoid process. This is the bone at the bottom of your sternum that serves as an attachment point to your rectus abdominus/ab muscle. My xiphoid process protrudes about 3 inches down into my abdomen - compared to the typical half inch. Although pain-free pre-pregnancy, I was a bit worried that this would become painful or be in the way with a growing abdomen (it never did).

Why we wanted to have an out-of-hospital birth
Philosophy
There ended up being many reasons for our decision to do a home birth. Kelton and I became friends with our eventual midwife Acadia Gantz via trail running about a year before getting pregnant. This was the first time either of us had talked with a midwife. We quickly learned that midwives like Acadia at Sacopee Midwives strive to provide an amazing (and therefore atypical) healthcare experience. We realized all of the similarities between her level of care and the care we strive to provide at our performance physical therapy clinic, Steady State. It became a no-brainer that we would work with her if we ended up getting pregnant.
It is increasingly more common that healthcare providers are choosing to have home births rather than birth in a hospital. We believe that this is because healthcare providers are the ones who experience daily all of the pains of treating people in an in-network (insurance based) setting. Treatments are decided based on whether or not insurance will cover it, and treatments are often pushed to be able to see a higher volume of patients. This goes for almost every in-network healthcare setting - and is a main reason why there are so many problems with the current standard healthcare.
One of the best resources I came across to emphasize these issues is the book “Babies Are Not Pizzas - They Are Born, Not Delivered” by Rebecca Decker. Rebecca is a mom & nurse who is able to provide an inside look at the politics of big hospital systems and the differences between a hospital birth and a home birth.
Birth is a natural process, not a medical event. For those who have higher risk pregnancies (including gestational diabetes, preeclampsia, placenta previa, or maternal health problems), hospitals are likely the safest place to give birth because more interventions may be necessary. Usually if there is going to be a complication during the birthing process there are signs and symptoms earlier on in the pregnancy that should be noticed by your healthcare provider.
As is typical in our current healthcare system - interventions are often pushed too early among those who remain low-risk throughout their pregnancy. Commonly pushed interventions for birth include epidurals, inductions, and C-sections. Many hospitals are continuously near capacity and therefore are not able to let the birth process last as long as it might naturally. A cascade of interventions can happen when there is a “failure to progress” which is when the hospital thinks that labor is taking longer than it should. Because they don’t have an endless number of birthing rooms - “failure to progress” is often diagnosed too early, which contributes to the C-section rate in the US being super high at roughly one-third. The recovery from a C-section from an orthopedic standpoint is significantly longer as your core is weakened from the surgical procedure. I knew that I wanted to do everything in my power to avoid a C-section to help my postpartum recovery!
Cost
Most people assume that working with a provider that is out-of-network with their insurance (cash-based) will be more expensive. However, it is very common for the opposite to be true.
We choose to have a lower monthly premium (a few hundred dollar monthly payment) and higher deductible (around $9k) health insurance marketplace plan because we are generally very healthy and we rarely need to see a medical professional. When we do, we prefer to pay for a higher level of service (and more time with the provider), which typically means the provider is already out-of-network. However, by having a "catastrophic" healthcare insurance plan in place we still would not have to pay more than our $9k deductible if we ever had a more serious medical emergency.
The average hospital birth cost in Maine is $6-9k WITH health insurance and $11-16k WITHOUT health insurance. Midwifery care was around half the cost it would have been if we had given birth in a hospital. The cost of working with our midwives also included all of our hour long prenatal and postnatal visits and being able to ask our providers questions via text/phone any time of day. Midwives truly are the bees knees!
Exercise During Pregnancy
Going into my pregnancy I was the fittest I had been since competing in Track & Field at the University of Maine 7 years prior. I was lifting & doing CrossFit 3 days a week and running up to 10 miles at a time.
I feel strongly that going into my pregnancy strong and durable allowed me to exercise more consistently throughout my pregnancy - which ultimately led to a successful and safe home birth. I was actually able to set a few lifetime lifting PR’s in the first trimester!
Throughout my 2nd trimester I was deadlifting weekly with my working sets being around 200 pounds. For reference, this was about 85% of my pre-pregnancy working set weight of 235#, based off a pre-pregnancy 1 rep max of 265#. Rather than focusing on how much weight I was moving my emphasis was listening to my body and adjusting accordingly each session.
Contrary to popular belief it is safe - and beneficial - to lift heavy during pregnancy. You don’t have to lift heavy or run during pregnancy but if you know what symptoms to look out for - and are not experiencing those symptoms - there is no reason to stop. This was one of my favorite things about my pregnancy: I didn’t stop doing things just because I was pregnant.
There are medical conditions where someone may be advised not to exercise at high intensities, however these situations are rare. Maybe I'll save "myths about exercise & pregnancy" for a future blog post.
My pregnancy ended up being low risk and therefore was quite uneventful. However I did have a two week stretch of pelvic girdle pain where I had to modify my running and get more serious with my prehab exercises. I also had significant heartburn that started early in my second trimester and only got worse. It was super frustrating that bending over to put my socks on felt worse than doing a heavy front squat! After running Beach to Beacon at 26 weeks pregnant, the jostling of stomach acid made running intolerable so I decided to hang up my running shoes for the third trimester.
Besides the heartburn I was surprised at how much I enjoyed being pregnant. I was fully expecting to be uncomfortable all of the time with back pain and pelvic pain. The bottom line is that you don’t have to accept aches and pains just because you are pregnant - strength training and rehab exercises can help!
Recovery Pillars: Sleep, Nutrition, Stress
Sleep
I had heard that it is common to get insomnia in the 3rd trimester, however I never had any issues sleeping. I used a pregnancy pillow in the second trimester to support my stomach when lying on my side, but by the 3rd trimester it was actually more comfortable to sleep without it and with just a regular pillow between my legs.
Nutrition
The number one question I was asked while pregnant was what my cravings were. Whole milk and milkshakes were my only consistent cravings!
I definitely experienced increased thirst and noticeably drank much more water. I did crave electrolytes throughout my pregnancy, which I consumed by adding Nuun tablets to a lot of my water.
I learned a lot of pregnancy specific nutritional information from the book Real Food for Pregnancy. The main thing I implemented was significantly increasing my egg intake for the added choline and protein.
I chose to cut my coffee intake from 3 cups per day to 1 cup in the morning. The research for eliminating caffeine altogether wasn’t strong enough for me to entirely kick my favorite beverage!
Stress
I didn’t have any significant added stressors from being pregnant, however there were a few things that were on my mind the whole time, including weighing our decision to have a home birth, the location of the birth (tiny house vs. my parents house vs. a birthing center), and not being in a hospital if something did go wrong.
When learning more about a home birth I learned that if there is going to be a complication at birth it is often predicted with monitoring the mother and baby throughout the pregnancy for risk factors. This knowledge helped tremendously with this fear, as well as knowing that we would be within a few minute drive of a hospital.
The Birth
End of pregnancy
During the end of my pregnancy I was pretty distracted from the final birth and baby prep. In the last 2 months we built a shed, had a baby shower, took a business trip to Atlanta, got covid, and the final week of my pregnancy we were busy at the clinic hosting our delayed grand opening party and onboarding our newest employee.
Living in a tiny house we don’t have space for a nursery for the baby, but we did clear a few spaces for his Moses basket, dresser, and changing station - which was all ready to go about a month before the due date.
Calix came 2 weeks early - so we were quite surprised when I started going into labor!
Early labor
Ironically, my first signs of early labor actually began while we were at our birth class at Birth Roots 3 days before labor. I didn’t know it at the time, but the low back pain that I was having while sitting in the class was likely one of my first symptoms. I had attributed it to commuting 2+ hours per day and less exercise during the previous 3 weeks since getting covid. Afterwards my mom noted that I seemed more agitated that weekend and our admin Farren told us "I knew something was off - that was the first time I heard you complain about being pregnant!”
The few days before the birth I was concerned there was something wrong. I was feeling less movement of the baby so I called Acadia for her to check things out. She listened to his heart beat and assured me that he was okay.
The day before Calix was born I saw clients the whole day - and ended the evening teaching one of our strength classes.
Active labor
Before giving birth I had 8 months to envision how I wanted my birth to go, but of course it always ends up a little different than planned!
I didn’t know that I was in labor until my water broke early Tuesday morning around 3 am. I woke Kelton up and he smiled and said “we’re going to have a baby today.” After cleaning up I grabbed a snack and tried to go back to bed. In hindsight I should have called my midwives to let them know - but I didn’t want to wake them.
I tried to fall back to sleep but I was nervous that my labor wouldn’t kick in naturally and that I would have to go to the hospital to be induced. Once your water breaks you no longer have a barrier from the outside world to your baby - so there is a risk of infection if you don’t deliver within 24 hours. I had my first contraction at 5:23. The next one came at 5:47 and then they fairly quickly became 5 minutes apart.
At 6am Kelton was offering breakfast but I couldn’t take in any food, so I settled on some sips of water. Not long after I started vomiting and shaking. Acadia arrived to check on me before we made the hour-long drive to my parent’s house. She discovered I was 3 cm dilated. Acadia later told me that she called Brenda (their other midwife on call) because she thought that I might be having the baby in the tiny house!
Kelton set up the backseat of the car with blankets and pillows and was frantically packing our things all morning. We hadn’t packed any bags yet!
We finally left the tiny house at 9:45. The ride was INTENSE. Luckily I had the handle and headrest of the seat in front of me to death grip. When we were 5 minutes away from my parent’s house we hit a road closure which forced Kelton to find another way around, adding on another 5 long minutes.
When we arrived Kelton helped me up to the shower. I thought that the warm water would help me relax and & ease the intensity of the contractions. I was only able to stand for one contraction - I didn’t feel like I had the strength to hold myself up and my legs felt shaky.
The active stage of labor was very different from what I had been envisioning. I was hoping to be more upright, mobile, and able to explore more positions. Instead I felt like I wasn’t able to move or hold my own body weight and my body demanded that I lay down.
The next hour I spent sidelying, alternating between a contraction and a few short minute long sleeps. By noon Acadia had arrived and performed another cervical exam and found that I was fully dilated and effaced - and ready to push!

Pushing
When my water broke earlier that morning I definitely did not think I'd already be starting to push my baby out only 9 hours later!
I was worried about having a really long labor so I mentally prepared myself for it to be long. So when it came to the pushing stage I thought to myself “holy shit the early part is already over.”
Pushing was what I was most excited about! I was looking forward to this stage because there is an end result - finally holding your baby.
I was not prepared for how strong the fetal ejection reflex would be. My body pushed without me trying for the first hour. It felt most natural to let my body take control.
Throughout the pushing I was encouraged to switch positions every 20 minutes or so. I switched between sidelying (using the rebozo as a pushing strategy by playing tug of war with Kelton), being on my hands & knees, sitting on the birth stool, and a half-kneeling lunge position leaning onto Kelton. This last position was the position I ended up birthing Calix in.
I didn’t get as much of a relief in between contractions as I thought I would. I felt like I needed something to hold me up - otherwise I felt unsteady. Acadia assured me that this was normal and due to the hormones.
The midwives listened to the baby’s heart rate during and in between contractions. In the last few contractions they noticed a drop in the baby’s heart rate and told me that they would have to do an episiotomy if I wasn’t able to push him out in the next contraction. This was the little extra motivation that I needed!
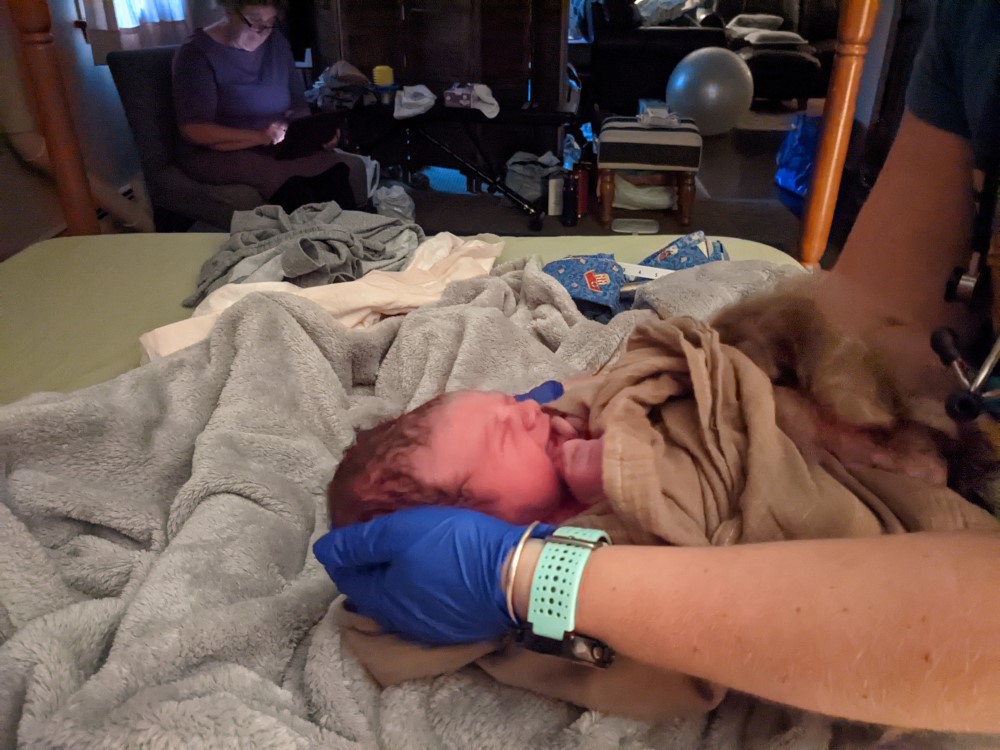
The next contraction came and I pushed as hard as I could. The contraction ended and the baby still hadn’t come out so I kept pushing. Finally Calix was born - not just his head but the whole body all at once!
Reflections
Ultimately we were very glad that we ended up going with a home birth. As I’ve reflected on the entire experience, I’ve only been able to think of positive things, which I’ve summarized below:
No interventions
It is super empowering to have birthed my baby without any interventions. With it being a home birth I didn’t even have an option for an epidural or other lines/tubes like an IV or catheter. Because of this I think I was better prepared mentally for the pain.
I also was able to avoid having a C-section. With my situation, if I had been in a hospital I would have started to get nervous that they may encourage a C-section after the first 2 hours of pushing. This could have easily led to me not being as relaxed and therefore fatiguing sooner - which likely could have led to the hospital staff recommending a C-section.
Pushing positions
Because I was able to avoid having an epidural, my pushing positions were limitless. I wasn’t attached to any lines or tubes and was able to move to the positions that felt the most productive.
Comforts of home & familiar faces
By not being in a hospital I didn’t have to be woken up every few hours to get my vitals taken and I could actually rest when my body needed it.
I knew exactly who my providers were beforehand and who was going to be in the room with me. I knew that an audience of strangers watching would likely slow things down for me.
Everything after the birth was exactly how we wanted
The newborn exam was done right in front of us on the bed after we were settled in. We were both able to do skin to skin without being rushed. Kelton was able to cut the cord. I wasn’t rushed to birth the placenta afterwards.
We didn’t have to get up to go anywhere for a full week. This was huge for me and allowed me to focus on my recovery and learning how to breastfeed. The original plan was to stay at my parents for 2-3 days, but we ended up staying for a week because I didn’t feel like I could comfortably go up and down the stairs into the sleeping loft in our tiny home, and sitting was still very uncomfortable. Having more options at my parent’s house was tremendously helpful.
Acadia came back to the home the day after the birth to check in. She then came to our tiny house for the 1 week follow up. We had a few more follow ups at home around 3 weeks and 6 weeks. During this time the midwives were also on-call for me and helped answer all of my new-mom questions & concerns.
Final thoughts
I’d recommend a home birth to anyone who remains low risk throughout their pregnancy who is looking for increased comfort, more individualized care, decreased medical expenses, and fewer medical interventions.
Throughout this blog post I’ve included links to most of the resources that I found the most helpful throughout my journey. I’ve repeated them all together below. My hope is that these resources and my positive birth story help anyone currently pregnant or considering getting pregnant.
I’m now 8 weeks postpartum and am continuing to see progress in my rehab. I’m looking forward to another post in the future where I’ll lay out my personal rehab story and my return to running & CrossFit.

If you have any questions or concerns or are looking for a pelvic health PT to assist you in your pregnancy or postpartum journey, please feel free to reach out. I can best be reached at ashten@steadystatehealth.com.
- Ashten
Resources
- Acadia Gantz, Brenda Surabian, Grace Pease
Naturopathic Doctor
- Dr. Karissa Deane at Luma Natural Health
Books
- Taking Charge of Your Fertility / fertility awareness method
- Babies Are Not Pizzas, They Are Born Not Delivered - Rebecca Decker.
- Expecting Better by Emily Oster
- Real Food for Pregnancy by Lily Nichols
- Ina May’s Guide to Childbirth by Ina May Gaskin
- Cribsheet by Emily Oster
Article
- Impact of heavy resistance training on pregnancy and postpartum health outcomes. (Prevett et al 2022)
Podcast
- The Happy Home Birth Podcast: Positive Birth Stories
Birth class