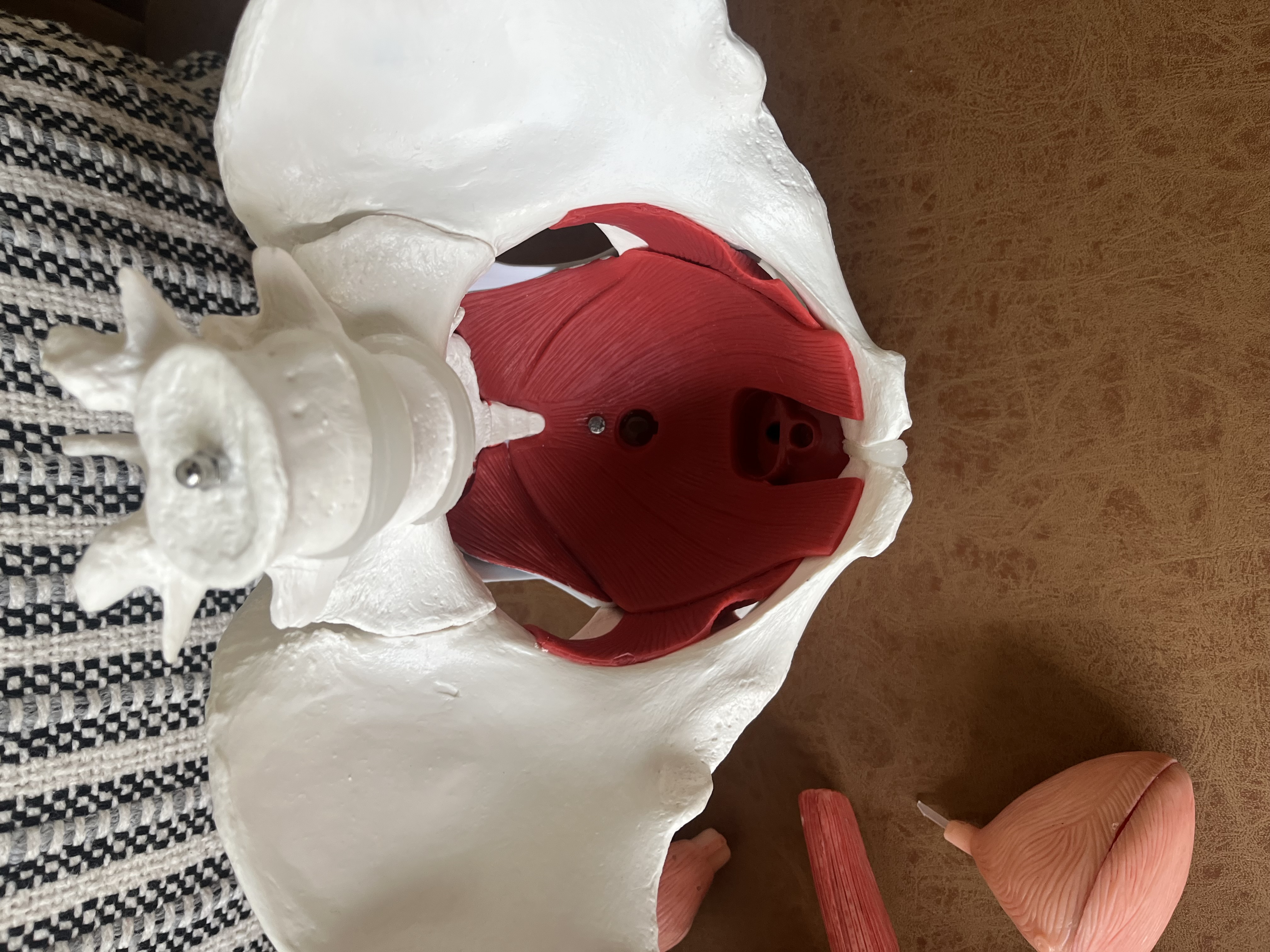
What is the pelvic floor?
How to Know if Pelvic Floor Physical Therapy is Right For You
Determining if you are a suitable candidate for pelvic floor physical therapy can indeed be a complex task, especially when conflicting advice may leave you uncertain about the normalcy of your experiences. Whether it's being told that a bit of postpartum leakage is typical or advised to unwind with a glass of wine for discomfort during intimacy, these doubts can persist. Perhaps you've convinced yourself that minor bladder issues run in the family or that lifelong constipation is standard. However, all of these concerns can be effectively addressed through pelvic floor physical therapy. This blog post aims to offer clarity on whether seeking help is the right course for you.
Pelvic floor conditions are often overlooked, dismissed, or considered a natural part of daily life by many. However, research indicates that these conditions are more prevalent than commonly believed. For instance, a study focusing on elite athletes discovered that out of 754 participants, 33% experienced urinary incontinence during their sports activities (Cite). This percentage was higher in high-impact sports like running and jumping. Another study (Cite) explored the correlation between low back pain and pelvic floor dysfunction, revealing that 95.3% of the 85 women studied had associated pelvic floor dysfunction.
Understanding that assistance is available if you are facing symptoms is crucial. Below, we've outlined common symptoms or conditions that would significantly benefit from pelvic floor physical therapy:
Urinary Incontinence (UI):There are three primary types of urinary incontinence, all of which can be effectively addressed through pelvic floor physical therapy:
- Stress incontinence: Leaking urine during moments of physical stress such as sneezing, coughing, laughing, lifting heavy objects, or running.
- Urge incontinence: Experiencing a sudden, intense urge to urinate even when the bladder isn't full.
- Mixed urinary incontinence: A combination of stress and urge incontinence. Pelvic floor physical therapy can effectively treat all three types.
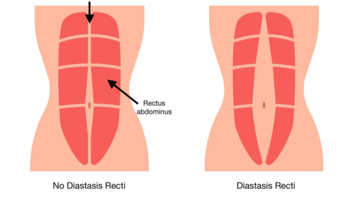
- This care is immensely beneficial in preparing the body for childbirth, offering education on birthing positions, symptom management, and maintaining a strong and active body throughout pregnancy. Postpartum pelvic floor physical therapy is valuable for individuals who have had a cesarean section or a vaginal birth. Birth injuries are common and can lead to debilitating symptoms that one does not need to endure. These injuries include tearing, episiotomies or surgical incisions, muscle avulsion, and pelvic organ prolapse. Regardless of the mode of delivery, scar tissue needs mobilization, and rebuilding pelvic floor and core strength is essential to return to beloved activities.
- This occurs when pelvic organs (bladder, uterus, urethra, rectum) descend into the vaginal canal. Symptoms may include a feeling of heaviness or as if something is protruding or dropping, accompanied by discomfort. Pelvic floor physical therapy focuses on symptom management, strength-building, and determining whether the individual would benefit from a support pessary (an assistive device akin to wearing a sports bra for chest support).
- This category encompasses conditions like erectile dysfunction, pain during intercourse (dyspareunia), and difficulty achieving orgasm. Given the multifaceted nature of these issues, a pelvic floor physical therapist can provide clarity on the next steps—whether that involves a personalized program or a referral to a specialist to address your specific needs.
- Individuals experiencing vulvar pain lasting more than three months (vulvodynia), involuntary contractions causing extreme vaginal tightness (vaginismus), endometriosis, bladder discomfort (interstitial cystitis), or general pelvic floor dysfunction could significantly benefit from pelvic floor physical therapy. Pain often creates hesitation to try new activities or alter routines due to fear of exacerbating it. Pelvic floor physical therapy can provide guidance and build confidence after addressing the root cause of the pain.
- Conservative care before surgery can greatly benefit in preparing the body for the upcoming procedure, potentially reducing recovery time and improving postoperative function (Cite). Various surgeries, including hernia repairs, hysterectomy, and any operation involving the abdomen and pelvis, may benefit from this approach. Depending on the specific surgery and individual circumstances, physical therapy can typically commence soon after the operation. The focus shifts with tissue healing timelines, aiming to address scar tissue and soft tissue mobility, rebuild pelvic floor and core strength, manage symptoms, and guide the individual back to their favorite activities through an individualized program.
If you have questions concerning any of the above listed categories or something not mentioned, feel free to reach out to us. If any of the above symptoms resonate with you, even without a diagnosis, that's okay—you don't need one to consult a pelvic floor physical therapist or initiate a discovery call with us. We can guide you through your next steps, whether that involves setting up an appointment or advising you to start by seeing a gynecologist, urologist, or another specialist.